The Whipple Procedure:
Life Saving Surgery for the Pancreatic Cancer Patient
Mom’s cancer is inoperable. Surgery is not an option.
BUT if it was, she’d be first in line for the Whipple Procedure. This is the name for the surgery that removes the cancerous pancreas. It’s a lot easier to say than the real name for the surgery:
Pancreaticoduodenectomy.
What a mouthful. Say that fast three times! I’ll stick with the Whipple, thank you very much. The nickname for this surgery comes from the man who worked to improve the surgical technique in the United States, Allan Whipple.
The idea has been around a long time, but the pancreas is a wily thing and difficult to remove successfully. Dr. Whipple refined the technique in 1935 and it’s been used with increasing degrees of success ever since. But make no mistake, it is still a major surgerical procedure often filled with complications. To understand why that is, let’s take a look at just how the Whipple Procedure is performed.
The Whipple surgery is, in mom’s words, basically re-plumbing your innerds. And she has that right. It is generally only an option if the cancer hasn't spread out of the pancreas and if the tumor hasn't compromised any of the major blood vessels. The Whipple Procedure is used for adenocarcinomas of the pancreas (those in the head of the pancreas). These pancreatic cancers account for roughly 95% of the cancer cases. Unfortunately, fewer than 10-15% of those patients are candidates for this surgery.
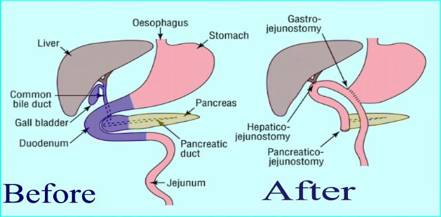
The Whipple surgery is generally divided into two stages: the Removal and the Reconstruction stages.
During the Removal Stage, the surgeon will “remove” (cut out) the following things:
- the head of the pancreas (and the cancer)
- the duodenum
-the gall bladder
- the common bile duct
-part of the stomach (usually, but not always)
-part of the small intestine (sometimes)
-the lymph glands in the area (sometimes)
That’s a lot of removing. And remember, the pancreas is a spongy, soft organ. It can be difficult to work with, making this surgery one requiring a very skilled surgeon who has extensive experience with the Whipple Procedure.
Once the cancerous portions are removed, the Reconstruction Stage of the surgery begins.
-generally the tail end of the pancreas, the hepatic duct (from the liver) and the remaining half of the stomach are sutured into the intestine so that food and digestive juices can pass through and be absorbed correctly.
- again, remember that the pancreas is that spongy, soft organ. It is difficult to suture back together and is one cause of the complications following the Whipple surgery.
Here’s a picture to help you visualize the procedure as simply as possible:
Recovery from all this re-plumbing will be tough, as you can imagine… You will probably spend the first day or so recovering from your Whipple Procedure in the intensive care. And don’t be surprised to wake up with lots of tubes sticking out of your body.
There will likely be Drain Tubes from your abdomen/stomach area to drain excess fluid, bile and/or pancreatic juice. Not pleasant, but necessary so that the fluid doesn’t collect inside your abdominal cavity. You do not want that…
In addition to these abdominal drain tubes, you might have a stomach tube. This tube is not always used, but can be very beneficial. It is a double-barrelled tube inserted into your stomach and small intestine draining out through your skin. It’s purpose is dual: to help drain fluid off the stomach and then as a way to administer high energy “food” to your small intestine, bypassing the stomach. You will not want Nausea and Vomiting to be a part of your vocabulary during the initial recovery. The stomach tube is all about keeping it that way.
You may also have a urinary catheter in place. Don’t worry, the surgeon didn’t mess with your bladder too. The catheter will be there for your comfort (yes, really), so that you won’t have to get up to go to the bathroom. Trust me, you won’t want to move at all for the first day or two…
The good thing about all these tubes, okay, I’m stretching the goooood thing here, is that they will be inserted/placed while you are still under anesthesia. You won’t feel a thing…. Until you wake up in intensive care. And remember, they are there to help with your recovery. The surgeon and/or nursing staff will be removing them as you heal.
And speaking of healing, the average hospital stage for a patient undergoing the Whipple procedure is 10 days-3 weeks, depending on your condition, the extent of the surgery and whether or not you have any complications.
Which leads right in to the nitty-gritty of this surgery: the complications.
In the early years of the Whipple, complications caused nearly a 25% mortality or death rate. Today, with advances and improvements in the technique, the mortality rate is below 5%. The complications and risks associated with the Whipple need to be weighed carefully before consenting to this surgery. The risks can be greatly reduced by choosing a surgeon who has vast experience with the Whipple procedure and has completed many of them successfully.
Still these are the most common complications you might experience:
1. Pacreatic Fistula – Remember how soft and spongy that pancreas is? Well, that consistency makes it very difficult to suture or stitch back into the intestine during the reconstruction stage. If the suture line doesn’t heal well, pancreatic juices can leak out into the abdominal cavity. Not a good thing. But that’s where the drainage tubes come in. They are there to “drain” off the juices. Yucky and uncomfortable, but worth the nuisance. In most cases, the leak heals on its own without requiring further surgeries.
2. Gastroparesis or Paralysis of the Stomach – to understand this complication, one must realize that the stomach and intestines are in a constant state of undulating movement, rolling the food right on down through the digestive system. During the Whipple Procedure, especially if half of the stomach is removed, these normal muscle movements stop or are paralyzed. Sometimes it takes awhile for the muscles to begin working again. Until they start working properly, food will just sit in your stomach, going nowhere (but back up). While this paralysis is relatively normal and to be expected, the surgeon can’t always say how long the gastroparesis will last. In some cases it can last 4-6 weeks. Whoa! That’s a long time! During which time you won’t be able to tolerate food on your stomach. Again, that’s where the wonderful tubes come in, especially that feeding tube placed during surgery into your small intestine. You will be “fed” high energy nutrition through the tube until your stomach begins to function again. There’s not a lot you can do to hurry this process up, but one thing that might help is to be as active as possible. Simply walking everyday may encourage the muscles to get moving too. This complication isn’t so much life-threatening as it is emotionally draining.
Hang in there… the up side is you’re not dealing with the nausea of pancreatic cancer anymore. Gastroparesis is a small price to pay for getting rid of the beast!
3. Finally, a long term complication of the Whipple Procedure would have to be Loss of Weight. I know, everything about pancreatic cancer ends in weight loss. Even the life-saving surgery! Go figure. But it’s understandable really. With the head of the pancreas removed, so are the important pancreatic digestive juices. This leads to mal-absorption of your food. In other words, your body just isn’t getting all the nutrients it needs to thrive. Eating smaller meals and frequent snacks helps as well as talking with your health care provider about taking a pancreatic enzyme replacement. Some think it helps, some don’t. Jury is still out on this subject. We all watched Steve Jobs lose weight after his reported Whipple surgery. The pancreas is a vital organ in our digestive system. Whether threatened by cancer or by surgery, we really don’t function at 100% without it.
The Whipple Procedure is not for the faint of heart. But if it can be an option in your pancreatic cancer journey, then Hallelujah! It is the only way to completely remove the cancerous tumor. I say that with a small caveat: even though the tumor may be successfully removed, experts still advocate pursuing follow-up chemotherapy. Those pancreatic cancer cells are insidious and small. Even when the surgeon removes all of the tumor he can see with his naked eye, there may be some nasty cells lurking in the shadow just waiting for their chance to dig in and grow. Don’t take that chance. Follow up with all your doctors recommendations.
Let the Whipple Procedure be the first step of the rest of your cancer-free life!
If you have a Whipple Surgery story to share we would be delighted to hear about it. While our research on the Whipple covered a lot of territory and is a good place to start, there is nothing like experiencing the real thing...
We would be honored if you would share your Whipple Surgery experience with us here.
Return to Treatment Options from the Whipple Procedure
Return to Home Page for the Pancreatic Cancer Journey
Copyright © PancreaticCancerJourney.com
Nothing on this website should be construed
to constitute medical advice.